Lightning Dental is publishing this recurring series based on real dental board complaints and disciplinary actions. It is designed to provide dentists with case studies and analysis that will ultimately help them reduce risk, strengthen documentation practices, and reduce exposure to potential dental board complaints.
Lightning Dental is publishing this recurring series based on real dental board complaints and disciplinary actions. It is designed to provide dentists with case studies and analysis that will ultimately help them reduce risk, strengthen documentation practices, and reduce exposure to potential dental board complaints.
Make sure to check our blog for future updates.
Case Study 1: Sedation Without Documented Caretaker Instructions
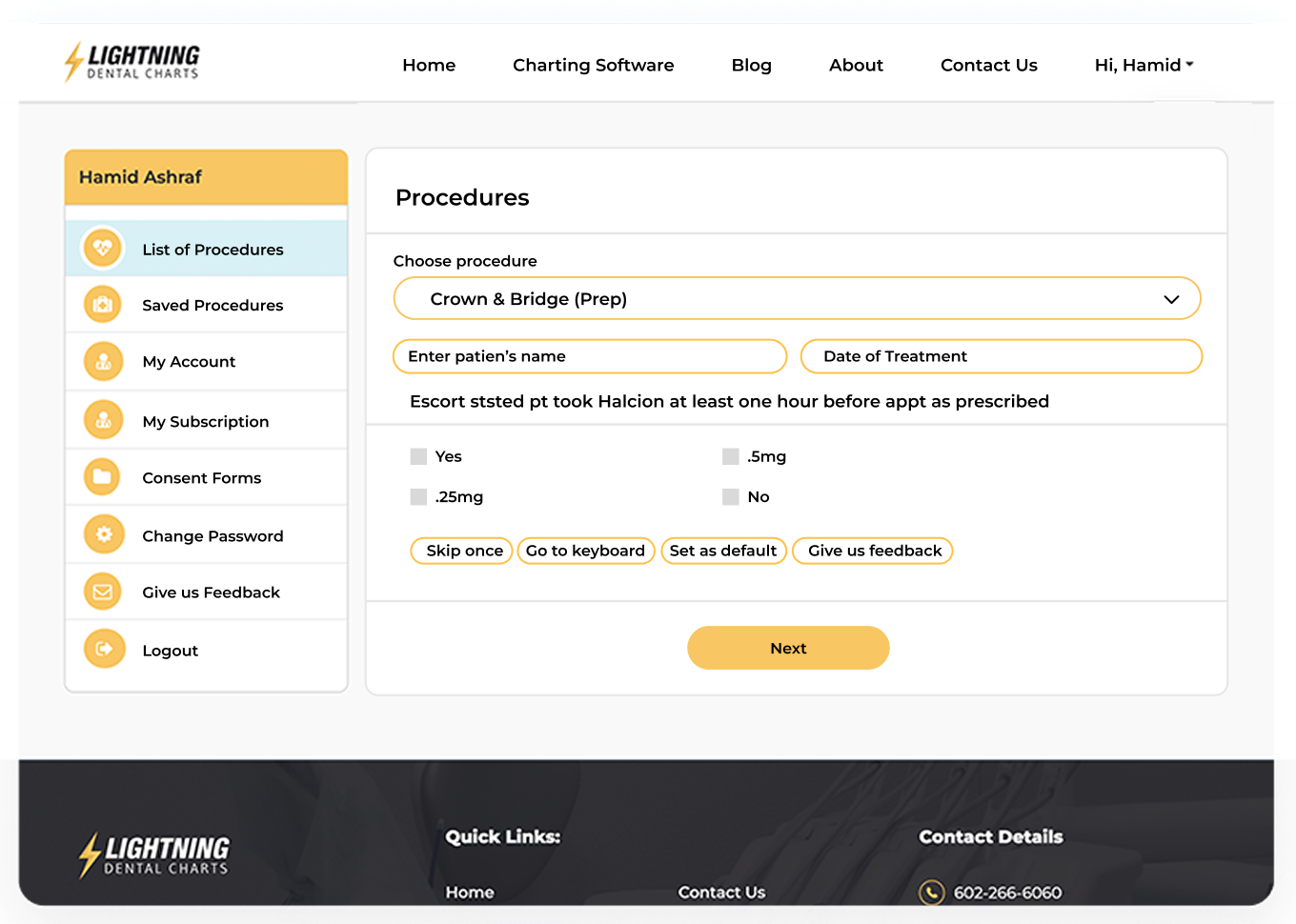
A sedated patient filed a complaint with the state dental board, claiming the practice allowed him to drive home while impaired. The dentist denied this, but the board looked for — and could not find — any documentation confirming that a caretaker or escort was instructed and present at discharge.
Most notably, there was no signed “Instructions for Escort/Caretaker” form in the progress note. Without proof of this standard-of-care safeguard, the board restricted the dentist’s sedation privileges.
Why This Matters
In all cases involving sedation — whether moderate, deep, or oral conscious — the burden is on the provider to confirm and properly document that the patient is discharged in a safe and compliant manner.
Failing to create and retain proof of caretaker instruction is not only a potential risk to patient safety. It also creates possible legal exposure that dental boards take seriously.
Key Takeaways
- Always use a signed escort/caretaker instruction form for all sedated patients.
- Include the form in your permanent records and reference it in your progress notes.
- Reinforce this step in your staff’s sedation discharge checklist.
Case Study 2: Unexpected RCTs and Over-Treatment Allegations
In another case, a dentist treatment planned 7 simple fillings. However, upon excavation, the dentist determined that 5 teeth required root canals or crowns. As a result of this major, unplanned escalation in care and cost, the patient was understandably upset and filed a board complaint.
When reviewing the complaint, the board examined the initial diagnostic radiographs and concluded that the original treatment plan may have underestimated the severity of decay. The lack of interim documentation — such as intra-oral photographs or progress note explanations — failed to support the dentist’s claim.
As a result, the board flagged the provider for over-treatment and poor documentation.
Best Practices for Elevated Diagnoses
Clinical judgment must often evolve once treatment begins. But when recommending a significantly more invasive or expensive treatment:
- Take intra-oral photos to support your clinical findings.
- Document the rationale for changing the treatment plan in your chart notes.
- Provide a clear explanation to the patient and update the consent accordingly.
Don’t Forget: Radiographic Guidelines Still Apply
Per ADA radiographic guidelines, initial x-rays should be detailed enough to support any diagnoses. If you find more extensive decay during treatment, update your radiographs and document the findings accordingly.
Case Study 3: Imaging Non-Compliance Triggers Fines
In a subpoena following a patient complaint, the dental board issued a subpoena for the dentist’s x-rays and imaging. However, the files the dentist’s office sent in response were not in the proper format. Several images failed to open and/or lacked visible date/time stamps.
The board cited the dentist for non-compliance with subpoena requirements and issued a $500 administrative fine.
What the Board Requires
Board subpoenas almost always include specific formatting rules or guidelines. In this case, the instructions stated:
“All images transmitted shall ONLY be in a JPEG or Adobe PDF format, clearly labeled with date/time stamp.”
Although this might seem trivial, such a requirement is not a technicality. It’s a compliance requirement. Overlooking such guidelines can lead to dental board censure or fine, even when the underlying treatment was sound.
Action Steps
- Confirm that all imaging systems export to JPEG or PDF.
- Always include date and time stamps.
- Store all original images in formats that meet board compliance guidelines.
Documentation = Defense
Across all three of these dental board cases, the board’s disciplinary action came down to one thing: documentation failures.
In today’s regulatory environment, the assumption is not that care was appropriate — it’s that if it’s not documented, it didn’t happen.
That’s why risk management for dentists now depends more than ever on:
- Accurate, timestamped imaging.
- Charting that reflects diagnostic logic.
- Pre- and post-operative documentation that protects both the patient and the dentist.
This is also why Lightning Dental Charts is the best dental charting software to help minimize dentists’ malpractice risk, while also helping unlock greater efficiency for their staff and practice.
Keep Learning: More from The Dental Board Report
We’re publishing real-world case studies from actual board complaints to help dentists strengthen their documentation and protect their licenses.
- Read our master article to understand how board reviewers evaluate records.
- Read the first sub-article in The Dental Board Report series.
- Check back regularly as we continue adding more insights to The Dental Board Report series.